Overactive Bladder (OAB)

Overactive bladder (OAB) is a common condition that affects millions of Americans. Overactive bladder isn’t a disease. It’s the name of a group of urinary symptoms.
SYMPTOMS
Urine Leakage: The most common symptom of OAB is the uncontrollable and sudden urge to urinate. Some people will leak urine when they feel the urge. Leaking urine is called “incontinence” or “urgency incontinence.” Some people may leak just a few drops of urine while others experience a sudden gushing of a large amount of urine.
Frequent Urination: Another symptom is the need to go to the bathroom many times during the day. The number of times someone urinates differs from person to person. But many experts agree that going to the bathroom more than 8 times in 24 hours is “frequent urination.”
Nighttime Urination: Having to wake from sleep to go to the bathroom more than once a night may be another symptom of OAB.
KEY STATISTICS
About 33 million Americans have overactive bladder. As many as 30% of men and 40% of women in the United States live with OAB symptoms. But the real number of people with OAB is most likely much larger because many people living with OAB don’t ask for help. Some are embarrassed and don’t know how to talk to their health care provider about their symptoms. Other people don’t ask for help because they think there aren’t any treatments for OAB.
EFFECTS OF OAB
OAB can get in the way of a person’s work, social life, exercise and sleep. Without treatment, OAB symptoms make it hard to get through the day without frequent trips to the bathroom. They may feel nervous about going out with friends or doing everyday activities because they are afraid a bathroom may not be close when needed. Some people begin to shy away from social events which leads to feelings of loneliness and isolation.
OAB may affect relationships with a spouse or family. It can also one of a good night’s sleep. When one is deprived of sleep, they will feel tired and depressed. Additionally, when a person leaks urine they may develop skin problems or infections.
WHAT TO DO?
If you think you may have OAB, call Rosemark Women Care Specialists and make an appointment with one of the gynecologists. The Rosemark gynecologists specialize in women’s health issues like OAB. Sometimes OAB symptoms are the result of a urinary tract infection, an illness, damage to nerves, or a side effect of a medication. So it’s important to call Rosemark for an appointment to identify the source of the problem and choose a treatment plan that is best for you.
How the Urinary Tract Works
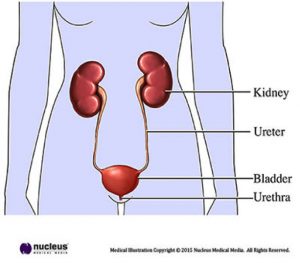
The bladder and kidneys are part of the urinary system the organs in our bodies that produce, store and pass urine. You have 2 kidneys that produce urine. Then urine is stored in the bladder. The muscles in the lower part of the abdomen hold the bladder in place.
When it isn’t full of urine, the bladder is relaxed. When nerve signals in the brain signal that the bladder is getting full, the need to urinate is felt. Normal urinary systems can delay urination for some time.
To begin urination, the brain sends a signal to the bladder. Then the bladder muscles squeeze or “contract.” This forces the urine out through the urethra, the tube that carries urine out of the body.
The urethra muscles, called “sphincters,” help keep the urethra closed so urine doesn’t leak before one is ready to urinate. These sphincters relax and open up when the bladder muscles contract.
OAB can be caused by the nerve signals between the bladder and brain signaling the bladder to empty even when it isn’t full. OAB can also be the result of bladder muscles being too active. In this case, the bladder muscles contract to pass urine before the bladder is full. This is what causes the sudden, strong need to urinate which we call “urgency.”
RISK FACTORS OF OAB

- As women age, the risk of OAB symptoms increases. But not all people will have signs of OAB. At any age, there are treatments that can help.
- Overactive bladder and urine leakage are not “normal” or expected parts of the aging process.
- Age doesn’t mean OAB symptoms can’t respond to treatment
- Both men and women are at risk for OAB. Women who have gone through menopause and men who have had prostate problems seem to be at greater risk for OAB.
- People with diseases that affect the brain or spinal cord, such as stroke and multiple sclerosis, are at high risk for OAB.
PHYSICAL EXAM
During a physical exam, the Rosemark gynecologists will ask a number of questions to understand a patient’s medical history including information about current OAB symptoms. The provider will want to know how long the symptoms have existed and how they are affecting lifestyle. A medical history will also include information about past and current health problems, prescription and over-the-counter medications, and diet including standard liquid consumption.
Once information about a patient’s history is completed, the provider will perform a physical examination to look for conditions that may be causing symptoms. In women, the physical exam will likely include an exam of the abdomen, pelvic organs and rectum. In men, a physical exam will include the abdomen, prostate, and rectum.
In some cases, a patient may be asked to keep a bladder diary, where the frequency of urination and leakage is documented. This will help the doctor learn more about day-to-day symptoms.
Other Tests
There are a few tests that the Rosemark gynecologists may order to help in the diagnosis and treatment plans of their patients. They include:
-
Urine culture:
A sample of urine to test for infection or blood.
-
Bladder scan:
An ultrasound that shows how much urine is still in the bladder after urination.
-
Cystoscopy:
A test where the doctor inserts a narrow tube with a tiny lens into the bladder so they can see the inside of the bladder.
-
Urodynamic testing:
A test that checks to see how well the lower urinary tract stores and releases urine.
-
Symptom Questionnaire:
Some of the Rosemark providers may use a written quiz to ask questions about bladder problems and what causes the most discomfort.
 There are a number of treatments the gynecologists at Rosemark Women Care Specialists may use to manage OAB including:
There are a number of treatments the gynecologists at Rosemark Women Care Specialists may use to manage OAB including:
- Lifestyle changes
- Medical and surgical treatments
- Managing leakage with products and devices
Since there is not a single treatment that is right for everyone, the Rosemark doctors may use one or more treatments alone or together. Based on all factors relating to the patient, the Rosemark provider will discuss treatment options that will best for the patient’s circumstance.