Osteoporosis

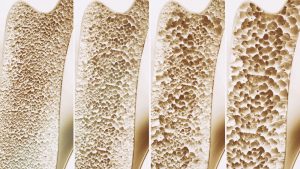
When bones become thin, brittle, and weak, osteoporosis may be the diagnosis. This change in bones can increase the risk of fractures which can lead to disability and even increase the risk of death.
Osteoporosis occurs five times more often in women than in men.
Osteoporosis may increase in severity after menopause because the female hormone, estrogen, decreases. Estrogen is a critical hormone to protect against bone loss and after menopause the ovaries produce very little of it.
The decrease in estrogen triggers a period of rapid bone loss in women that starts one year before the final menstrual period and can last up to 3 years. In addition, the natural effects of aging on bones can lead to bone loss as well.
CONTRIBUTING FACTORS
Factors that can cause or contribute to osteoporosis and fractures:
- Certain medications such as Prednisone, Femara, Prevacid, Depo Provera and others
- Diseases such as inflammatory bowel disease, rheumatoid arthritis, and lupus
- Low calcium
- Low Vitamin D
- High amounts of vitamin A
- High caffeine intake
- Too much salt in your diet
- Three or more drinks of alcohol per day
- Being immobile or not having adequate physical activity
- Active or passive smoking
Osteoporosis may not cause any symptoms for many years. Signs and symptoms do occur as the disease progresses. As the vertebrae in your spine weaken, they can fracture. Fracture in the front part of the spinal bones can result in loss of height or curving of the spine. This type of spinal fracture often causes no pain. Sometimes, fractures of the spine can cause pain that travels.
BONE DENSITY TESTS

A bone mineral density (BMD) test is where the bone density is measured at the heel, spine, hip, hand, or wrist. Several types of BMD tests are available. Rosemark offers the Dual-energy X-ray absorptiometry (DXA) of the hip and spine which is considered to be the most accurate bone mineral density test available.
At Rosemark we begin bone density testing at age 65 or earlier if there’s certain risk factors or after menopause regardless if the menopause is natural or surgical. Women who are younger than 50 years and are post-menopausal should have a BMD test if:
- A bone fracture has occurred
- Other risk factors for osteoporosis exist, such as rheumatoid arthritis, smoking, alcoholism, a history of hip fracture in a parent, or a body weight less than 127 pounds.
During a DXA scan, the patient lies down for 3–10 minutes while a machine scans their body. With this test the patient is exposed to a small amount of radiation, less than the amount in a normal chest X-ray.
T-Scores
After the test, a T-score is given for each site measured. A negative score means that bones are thinner than an average 30-year-old woman. A positive score means that bones are stronger than an average 30-year-old woman. If the T-score at any site is -1 to -2.5, it is considered low BMD and the patient has an increased risk of osteoporosis. A score of -2.5 or lower means that the patient has osteoporosis. Treatment usually is recommended to prevent fractures.
BMD Test Frequency
The frequency of BMD testing depends on age and results of previous DXA scans. Women 65 years and older with normal bone mass or mild bone loss should have a test every 15 years.
More frequent testing is recommended for women with T-scores between -1.5 and -2.49. Generally every 2 years a BMD will be done if osteoporosis is diagnosed and may be earlier if it is warranted.
FRAX is a tool used to estimate fracture risk. It is part of the results provided when a Rosemark bone mineral density test is completed. The FRAX program helps predict the risk of having a fracture within the next 10 years in women aged 40 years and older who are not taking prescription osteoporosis drugs.
OSTEOPOROSIS MEDICATIONS
Various medications are used to treat osteoporosis and help reduce the risk of fractures. Bisphosphonates increase bone mineral density by slowing down the rate at which osteoclasts break down bone. Some bisphosphonates are oral. Alendronate and Ibandronate may be taken orally or by IV but only women can take this medication.
Another option may be Calcitonin, which is a hormone naturally produced by the thyroid. Calcitonin produces a modest increase in bone mass because it slows down the rate of the osteoclasts.
Treatment with Estrogen hormone therapy is another option. Your Rosemark provider will evaluate an individual’s specific medical history and bone loss. Depending on the evaluation from a physician, a treatment plan will be established to help reach the best increase in bone density.
LIFESTYLE AND OSTEOPOROSIS
Lifestyle plays a key role in preventing osteoporosis. Exercise increases bone mass before menopause and slows bone loss after menopause. Bone is living tissue and exercise makes it grow stronger.
A healthy diet with calcium rich foods, and not smoking, help keep bones strong and healthy throughout a person’s lifetime. It is never too early to start thinking about bone health. Good bone health should start during childhood. This is the time to focus on building and keeping as much bone as possible through exercise, good nutrition, and healthy living.
Calcium
Calcium is important to building and maintaining healthy bones. Vitamin D helps the body absorb calcium. To increase your daily levels of calcium, eat a variety of calcium-rich foods. Good sources of calcium include dairy products like yogurt, milk, cheese and ice cream; dark, leafy greens, like spinach, kale, and collards; and canned fish with soft bones, including salmon and sardines. Intake of Vitamin D can increase levels by eating foods fortified with Vitamin D. Another great resources for Vitamin D is the sun and good Vitamin D supplements.
If you are concerned about osteoporosis, contact our office for an appointment to discuss your condition with one of our expert health care providers.